What Is a Total Hysterectomy? Key Facts & Recovery


If you’re searching for ‘total hysterectomy,’ you’re likely seeking clarity about this significant surgical procedure. A total hysterectomy involves the complete removal of your uterus to treat conditions like cancer or severe endometriosis. This article demystifies the process, outlines recovery expectations, and considers long-term impacts, equipping you with knowledge to make informed decisions about your health.
Key Takeaways
A total hysterectomy is the surgical removal of the entire uterus including the cervix, with varying types such as abdominal, vaginal, laparoscopic, and radical hysterectomies, each with their own approach and recovery times.
Reasons for undergoing a total hysterectomy include severe health conditions like various cancers, adenomyosis, uterine fibroids, and persistent heavy menstrual bleeding; less invasive treatments or conservative management may be considered before opting for surgery.
Recovery from total hysterectomy generally takes 6 to 8 weeks and can involve immediate menopause symptoms if ovaries are removed; long-term effects include risk of heart disease, osteoporosis, and potential changes in sexual function, as well as emotional and psychological considerations.
What Is a Total Hysterectomy?
A total hysterectomy is a surgery that removes both the uterus and cervix. In some cases, the surgeon may also remove the ovaries and fallopian tubes—a procedure called a salpingo-oophorectomy. This is different from a subtotal hysterectomy, where the cervix is left in place. Hysterectomies are done to treat conditions like fibroids, endometriosis, or cancer.
After surgery, you’ll no longer have periods or be able to get pregnant. Recovery takes time—most people need several weeks to heal. Understanding the types, risks, and benefits can help you prepare for this life-changing procedure.
Understanding the scope of a hysterectomy is crucial, as it impacts both the surgical approach and the recovery process. Various types of hysterectomy surgeries exist, including:
Abdominal hysterectomy
Vaginal hysterectomy
Laparoscopic hysterectomy
Radical hysterectomy
Each type has its unique method and recovery timeline.
The Surgical Procedure of Total Hysterectomy

The surgical procedure of a total hysterectomy can vary depending on the individual’s health condition and the surgeon’s expertise. However, it generally involves the complete removal of the uterus and cervix.
The surgical process can be broadly divided into two main approaches - the abdominal hysterectomy and the vaginal or laparoscopic hysterectomy. These methods differ in the surgical technique, recovery time, and potential complications, which we’ll explore in the following subsections.
Abdominal Hysterectomy Approach
An abdominal hysterectomy is a traditional method that involves:
a 6 to 12-inch incision in the lower abdomen
direct access to the uterus and surrounding organs
facilitating the removal of large fibroids or addressing extensive endometriosis.
The recovery from an abdominal hysterectomy tends to be longer than other types, with patients typically requiring a hospital stay of two to three days. Despite the longer recovery time, this approach is often employed when the uterus is enlarged, or there is the need for comprehensive exploration of the pelvic cavity.
Vaginal or Laparoscopic Hysterectomy Techniques
On the other hand, vaginal and laparoscopic hysterectomies, which involve the removal of the uterus through the vaginal canal, are minimally invasive techniques that often lead to a quicker recovery and may help alleviate certain symptoms such as vaginal dryness.
In a vaginal hysterectomy:
The uterus is removed through the vagina
The patient lies on their back during the surgery
This method often results in a shorter hospital stay and lower cost.
A laparoscopic or robotic hysterectomy surgery involves using a laparoscope and small abdominal incisions to remove the uterus. This technique is particularly beneficial when there is scar tissue on the pelvic organs. Patients often experience less blood loss and shorter hospital stays with these minimally invasive techniques.
Reasons for Undergoing a Total Hysterectomy
Several health conditions might necessitate a total hysterectomy. These include:
Cervical cancer
Ovarian cancer
Fallopian tube cancer
Uterine cancer, particularly in advanced stages
In addition, adenomyosis, which is the growth of endometrial tissue within the muscle wall of the uterus, can lead to severe pain, necessitating a hysterectomy after other treatment options have been exhausted.
Uterine fibroids, benign tumors within the uterus, can lead to a hysterectomy when they cause heavy periods, pelvic pressure, frequent urination, and lower back pain. These fibroids can also result in heavy or painful menstruation, pelvic pain, and discomfort during intercourse, which are symptoms often treated with a hysterectomy when other therapies fail.
Persistent heavy menstrual bleeding, particularly when it is not mitigated by other treatments, may necessitate a hysterectomy. Abnormal uterine bleeding can also lead to a hysterectomy. This bleeding can manifest as heavy or prolonged menstruation or heavy vaginal bleeding due to various causes like ovulation issues or hormonal changes.
Recovery Journey After Total Hysterectomy

The recovery journey after a total hysterectomy involves both physical healing and psychological adjustment. Complete recovery typically takes 6 to 8 weeks, with the abdominal hysterectomy requiring the most time, and vaginal or laparoscopic hysterectomy requiring about 3 to 4 weeks.
During this recovery period, patients are advised not to lift heavy objects, but walking is often encouraged as part of the recovery process. Patients may also experience bloating, gassiness, and disturbances in bowel and bladder function, including constipation, which is occassionally experienced following abdominal surgery.
The following subsections delve into the specifics of hospital stay and initial recovery, along with home care and activity resumption.
Hospital Stay and Initial Recovery

The immediate period after a total hysterectomy involves:
A hospital stay, typically ranging from one to two days, though some may require a longer stay depending on their health condition and surgical approach
Medication for pain management
Support as needed
Laxatives and/or cathartics to treat or prevent constipation
Moreover, patients are encouraged to begin moving as soon as possible following the procedure to facilitate recovery. Early ambulation helps reduce the risk of blood clots, encourages bowel and lung function, and promotes faster healing.
Home Care and Activity Resumption
Once discharged from the hospital, home care becomes crucial for a smooth recovery. Patients should refrain from lifting heavy objects for four to six weeks following a hysterectomy to allow proper healing. Sexual intercourse should also be avoided until the surgical scars have healed and the vaginal discharge has stopped, typically a period of four to six weeks.
Patients may resume driving when comfortable wearing a seatbelt and can perform an emergency stop without discomfort, usually between 2 to 6 weeks after the surgery. Vaginal discharge is expected to last up to 6 weeks post-hysterectomy, with the amount being less than that of a typical menstrual period.
Long-Term Health Implications

Total hysterectomy comes with long-term health implications that every woman should be aware of before making the decision. Women who undergo a total hysterectomy and have their ovaries removed are likely to experience immediate menopause symptoms, such as hot flashes and mood swings. Even if the ovaries are not removed, some women may face early menopause due to compromised blood supply to the ovaries during a total hysterectomy.
Further, women might experience pelvic floor disorders such as stress urinary incontinence, vaginal vault prolapse, and uterine prolapse after a hysterectomy. On the other hand, women experiencing stress incontinence and/or prolapse prior to surgery can undergo repair of these conditions along with a hysterectomy. Moreover, undergoing a hysterectomy, particularly in cases involving the removal of ovaries, can lead to an elevated risk of heart disease and osteoporosis.
Life After Total Hysterectomy
Life after a total hysterectomy may involve both physical and emotional adjustments. Some patients may experience a loss of sexual desire, but it generally returns after full recovery. However, hysterectomy can lead to decreased libido and altered orgasm sensation, potentially due to nerve damage during surgery.
If the cervix is removed during a total hysterectomy, regular Pap tests may be necessary to monitor for any abnormal cells that could indicate the presence of cervical cancer. After a hysterectomy, particularly when the ovaries are removed, hormone replacement therapy may be considered to manage menopausal symptoms resulting from lower hormone levels.
Emotional and Psychological Considerations

A total hysterectomy can also have emotional and psychological implications. It may trigger feelings of sadness and loss due to the end of a woman’s childbearing years, even in those who did not desire children. On the other hand, emotional reactions to a hysterectomy can vary depending on the individual’s preparation for surgery, the reason for the surgery, and treatment outcomes, potentially leading to relief from chronic pain.
Support systems, counseling, and open discussions with healthcare providers about emotional concerns post-hysterectomy can mitigate negative emotional impacts. Engaging in self-care and femininity-affirming activities may assist with emotional recovery. However, some patients may experience a variety of emotional and psychological distress, such as:
a sensation of lack of control
pre-existing emotional issues
depression
a decrease in libido or sexual sensation
It is important to address these concerns and seek appropriate support and treatment if needed.
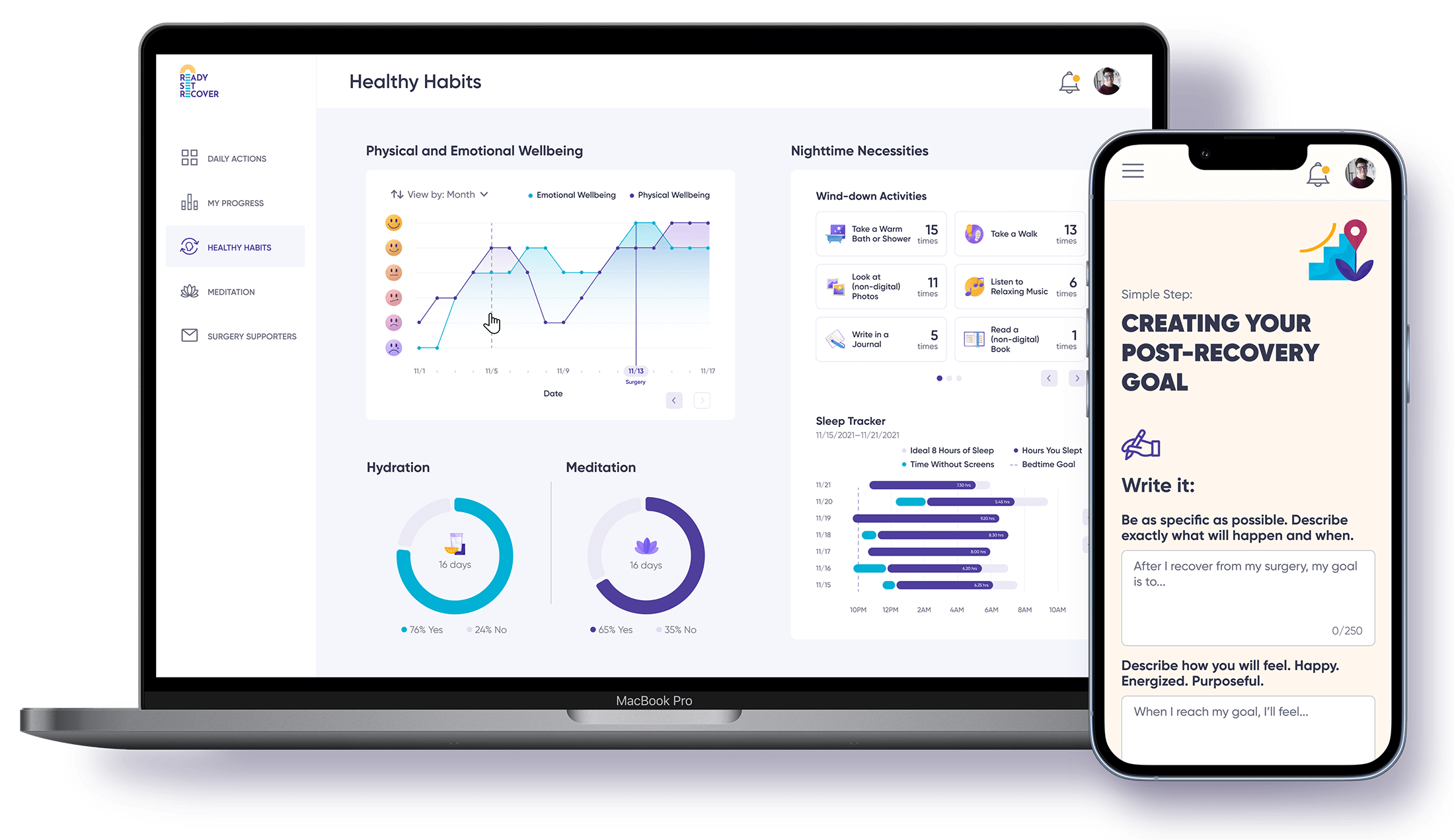
If you’re considering this procedure, you may also want to consider using Ready Set Recover to help you navigate the pre and post surgical challenges you may face so that you can be prepared and recover with more ease.
Alternatives and Complementary Treatments

While a total hysterectomy can be a life-saving procedure for some, it’s important to know that alternatives and complementary treatments exist. Less invasive surgical alternatives include:
Myomectomy for fibroid removal
Endometrial ablation
Uterine artery embolization
Laparoscopic procedures
Supracervical or subtotal hysterectomy only removes the upper part of the uterus and keeps the cervix intact, offering a less invasive surgical option than total hysterectomy.
Medications, such as iron supplements for symptoms of menorrhagia, and hormonal treatments with estrogen or progesterone, offer non-surgical options to treat conditions potentially leading to a hysterectomy. Moreover, recent studies suggest that removing only the fallopian tubes and keeping the ovaries during a hysterectomy could decrease the risk for the most common type of ovarian cancer, impacting the decision-making on ovarian conservation.
Patients should have thorough discussions with their doctors about all available options, understanding risks, benefits, and alternatives before deciding to undergo a major surgery like hysterectomy. There are also programs like Ready Set Recover that guide people in their pre and post total hysterectomy surgical journey.
Your Healing Journey: Life After a Total Hysterectomy
Total hysterectomy is a major surgery that can significantly impact a woman’s life. It involves the removal of the entire uterus and potentially other reproductive organs. The procedure is performed for various reasons, such as different types of cancers, adenomyosis, uterine prolapse, uterine fibroids, and persistent heavy menstrual bleeding.
The recovery journey varies depending on the surgical approach, but typically takes 6 to 8 weeks. Long-term health implications include early menopause, pelvic floor disorders, and increased risk of heart disease and osteoporosis. Life after a hysterectomy may involve changes in sexual desire, altered orgasm sensation, and the need for regular Pap tests if the cervix was removed. Emotional and psychological considerations also play a significant role, and it’s crucial to have a robust support system and counseling if needed. However, alternatives and complementary treatments to total hysterectomy exist, and it’s important to discuss these with healthcare providers before making a decision.
Frequently Asked Questions
What happens when you have a total hysterectomy?
After a total hysterectomy, the entire uterus along with ovaries and tubes and cervix are removed. This procedure is preferred over a subtotal hysterectomy to eliminate the risk of developing cervical cancer in the future.
What is the difference between a total and complete hysterectomy?
A total hysterectomy involves removing the entire uterus including the cervix. A complete hysterectomy, also known as a radical hysterectomy, goes further by removing the entire uterus, cervix, surrounding tissues, and parts of the vagina. In summary, a total hysterectomy removes the uterus and cervix, while a complete hysterectomy also removes surrounding tissues and part of the vagina.
What happens if you've had a full hysterectomy?
After a full hysterectomy, you will no longer have periods or be able to get pregnant. However, your ovaries may still produce hormones, so you may not experience other menopausal symptoms. Nonetheless, you may experience hot flashes due to blocked blood flow to the ovaries.
What are the reasons for undergoing a total hysterectomy?
Undergoing a total hysterectomy may be necessary due to conditions such as cancers, adenomyosis, uterine prolapse, fibroids, and persistent heavy menstrual bleeding. These conditions may require removal of the uterus for treatment.
What is the negative side of having a hysterectomy?
A hysterectomy can lead to hormonal changes, early menopause (if the ovaries are removed), and potential emotional effects like depression or a sense of loss. There’s also a risk of complications such as infection, blood clots, and pelvic organ prolapse over time.