Understanding Different Spinal Surgeries and What They Entail: Exploring Your Options


Are you considering spinal surgeries for your back pain or a diagnosed condition? Gain insight into the different types of spinal surgeries, their effectiveness for various spinal issues, and the recovery journey you might expect—all without wading through jargon.
Key Takeaways
Minimally invasive spine surgery offers numerous advantages, including reduced muscle damage, lower infection rates, and quicker recovery, with a high success rate of 90% in procedures.
Surgical interventions are effective for common spinal conditions such as herniated discs, spinal stenosis, and degenerative disc disease, with various surgeries like microdiscectomy, laminectomy, and discectomy improving patient quality of life.
Proper pre-surgery preparation is essential, including stopping certain medications and adjusting diet, while post-surgery recovery involves careful pain management and may require a personalized recovery plan to optimize outcomes. Learn more about what foods to eat after surgery.
Deciphering the Need for Spinal Surgery
The decision to undergo spinal surgery is influenced by multiple factors, paramount among these being the severity and nature of the spinal condition. Nevertheless, exploring non-surgical treatments like physical therapy should be the first course of action. These techniques often demonstrate effectiveness in controlled trials and can lead to improvement in many spinal conditions without the need for surgical intervention.
Before deciding on spinal surgery, you should consider several key factors such as:
Securing an accurate diagnosis with the use of an MRI or CT scan
Whether pain will resolve over a given time period
Whether there is an associated distal nerve weakness or paralysis from a ruptured disc
Weighing the cost of the operation
Gauging its potential impact on your lifestyle
Adequately preparing yourself mentally for surgery
This becomes especially crucial when experiencing neck pain, as the neck houses important structures like the spinal cord and nerves that can be affected by surgery.
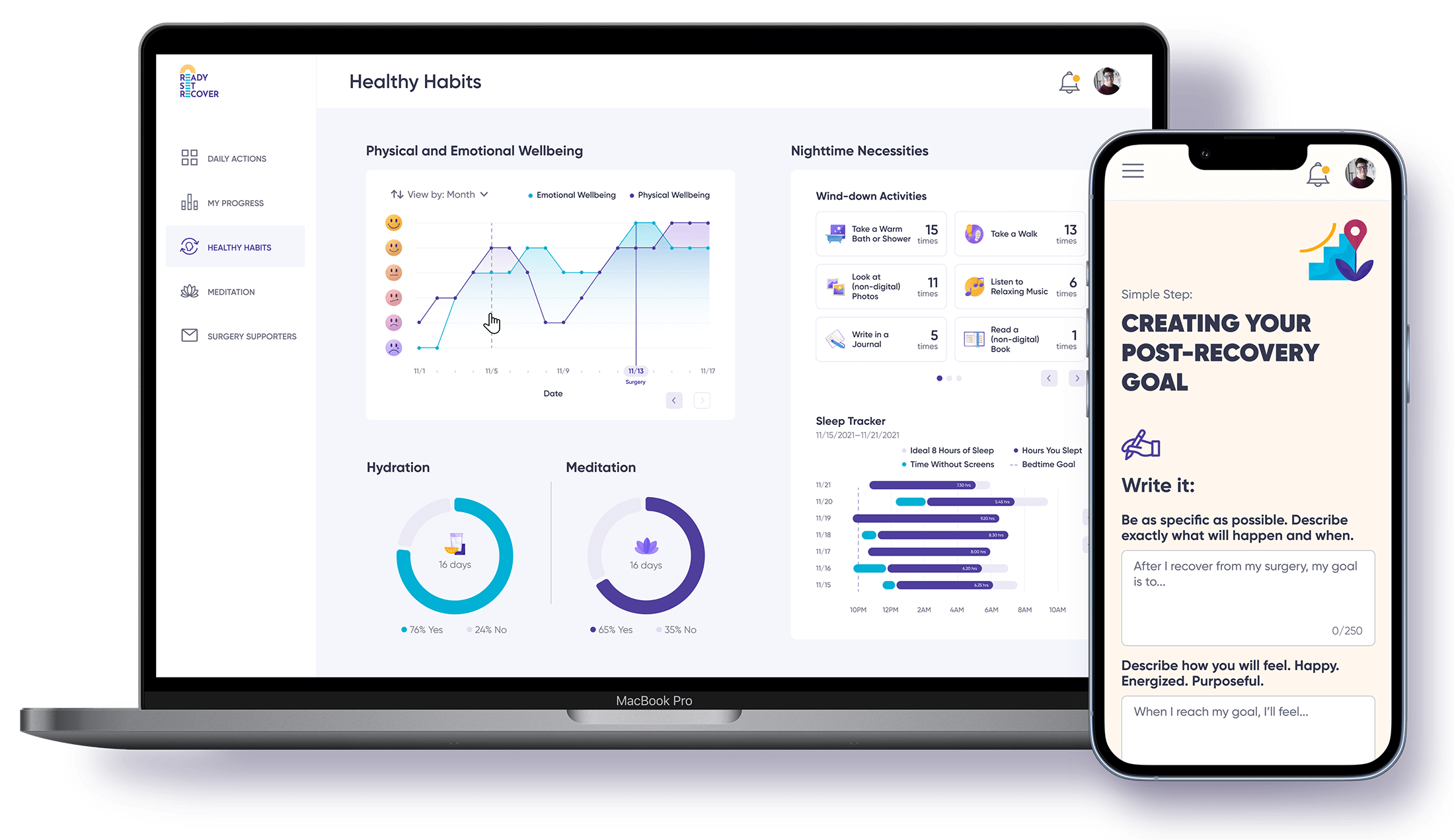
Grasping the structural causes of back pain is equally significant. These can range from:
Injury to muscles or ligaments
Inflammatory disorders
Malignancy
Pregnancy
Trauma
Osteoporosis
Nerve root compression
Radiculopathy: This is a condition caused by compression, inflammation and/or injury to a spinal nerve root.
Plexopathy: This is a disorder affecting a network of nerves. It often refers to brachial plexopathy (affecting the nerves in the arms and hands) or lumbosacral plexopathy (affecting the nerves in the lower back and legs).
Degenerative disc disease
Disc damage
Arthritis
Scoliosis
Poor posture
Bone spurs
Understanding these structural factors can help in identifying the most appropriate treatment.
Overview of Minimally Invasive Spine Surgery Techniques

Minimally invasive spine surgery, a groundbreaking advancement in medical science, has revolutionized the field of spinal treatments, including spine surgeries. This technique offers numerous advantages over traditional methods, such as:
Decreased risk of muscle damage
Lower infection rates
Reduced postoperative pain
Faster recovery period
Not only does this method minimize the physical impact on the patient, but it also optimizes the recovery process and enhances the overall patient experience. This is achieved through the use of advanced surgical techniques and state-of-the-art technology, which allows for precision and control during the operation. The end result is a procedure that is less traumatic for the patient, leading to improved outcomes and a higher quality of life post-surgery. It's important to note that while minimally invasive spine surgery has many benefits, it's not suitable for all patients or all types of spinal conditions. Therefore, it's crucial to have a thorough discussion with your healthcare provider to determine the best treatment plan for your specific needs.
Patients undergoing minimally invasive spine surgery generally experience the following benefits:
Less need for rehabilitation
Decreased reliance on pain medications
Perception of being less invasive, which contributes to its positive reception among patients.
Worth mentioning is the high success rate of minimally invasive spine surgery, with positive outcomes in approximately 90 percent of procedures. This impressive figure further highlights the effectiveness of these techniques.
Learn more about the minimally invasive Intracept Procedure for back pain relief.
Addressing Common Spinal Conditions Through Surgery
Several spinal conditions may necessitate surgical intervention. Prevalent among these are herniated discs, spinal stenosis, and degenerative disc disease.
Herniated discs often pose a significant source of pain and discomfort. Herniated disc surgery, which may involve procedures such as microdiscectomy or discectomy, is aimed at alleviating this discomfort. These surgeries involve the removal of the portion of the disc that is causing pressure on the nerve, ultimately providing relief from the chronic pain and numbness often associated with this condition.
Spinal stenosis, characterized by the narrowing of the spinal canal, is another condition that may require surgical intervention. Often, a laminectomy is performed to alleviate nerve pressure. This procedure involves the removal of the lamina, the back part of the vertebra that covers your spinal canal. This enlargement of the spinal canal can help reduce the pressure on the nerves and spinal cord, providing significant relief from symptoms.
For degenerative disc disease, a discectomy to eliminate the herniated disc is frequently employed. This procedure can significantly reduce pain and improve the quality of life for patients. It involves the removal of the disc material that is pressing on the spinal cord or nerve root, helping to restore normal function and movement while reducing pain. It's important to note that these surgeries are typically considered after conservative treatments have been tried and failed to provide adequate relief.
Studies indicate that surgical interventions, including minimally invasive procedures, effectively treat herniated discs, spinal stenosis, and degenerative disc disease. This further reinforces the rationale behind opting for spinal surgery for these conditions.
The Journey to Spinal Fusion: When and Why It's Done
When considering types of spine surgery, spinal fusion back surgery is a specific type of procedure aimed at reinforcing the structural integrity and stability of the back. By doing so, spinal fusion permanently connects two vertebrae, which involves the removal of bone and diseased tissues that may be causing pressure on spinal nerves.
Spinal fusion surgery is generally recommended for conditions such as spinal stenosis, spinal fractures, spinal deformities, spinal instability, and chronic back pain in patients.
Spinal stenosis, a condition where the spaces within your spine narrow, can put pressure on the nerves that travel through the spine, resulting in pain, numbness, or muscle weakness. Spinal fusion surgery can help alleviate these symptoms by creating more space for the nerves.
Spinal fractures can occur due to trauma or conditions like osteoporosis. These fractures can lead to severe back pain or neurological problems if the broken vertebrae impinge on the spinal cord. In such cases, spinal fusion surgery can help stabilize the spine and alleviate symptoms.
Spinal deformities such as scoliosis or kyphosis can lead to severe back pain, difficulty breathing, and other health problems if left untreated. Spinal fusion surgery can correct these deformities and relieve these symptoms, improving the patient's quality of life.
Spinal instability, where there is abnormal movement between two vertebrae, can lead to pain and nerve damage. Spinal fusion surgery can provide the necessary stability to the spine, preventing these abnormal movements and their associated symptoms.
Chronic back pain can have a significant impact on a patient's daily life, making it difficult to perform routine tasks. If conservative treatments fail to provide relief, spinal fusion surgery can be an effective treatment option. By eliminating the movement at the painful vertebral segment, it can provide long-term pain relief.
One should bear in mind that spinal fusion surgery stands apart from other spinal surgeries. Unlike many other procedures, spinal fusion aims to alleviate pain caused by the movement of vertebrae by connecting two adjacent ones and thus limiting their movement.
Pre-surgery Preparation
Proper preparation before spinal surgery is key to achieving a successful outcome. One key aspect is proper medication management. For instance, it’s advisable to discontinue the use of medications containing aspirin for at least 7 days prior to spinal surgery, as these can increase the risk of bleeding and complications involving the spinal cord.
Dietary modifications are also recommended in the week leading up to the surgery. It’s beneficial to reduce the consumption of red meat and instead focus on incorporating a high-fiber diet from fruits, vegetables, beans, and whole-grain cereals.
Maintaining physical fitness prior to surgery is vital for:
Improved post-operation outcomes
Increased pain relief
Heightened patient satisfaction
Better mental health
Creating a spine-specific recovery trajectory, facilitating a smoother recovery process.
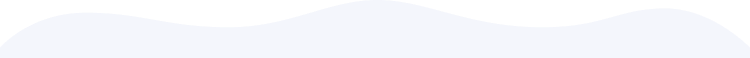
In addition to these steps, using a program like Ready Set Recover can significantly enhance your preparation for surgery and optimize your recovery process. Ready Set Recover is a comprehensive program that provides tools and resources to help patients prepare for surgery, manage their recovery, and achieve the best possible outcomes. The program includes action steps, educational materials, and a deep level of support during a difficult time. By using Ready Set Recover, patients can feel more confident and empowered in their journey toward recovery.
Post-Surgery Pathways: Pain Management and Recovery

After surgery, effective pain management becomes a vital part of recovery. Typical strategies include the use of medications like opioids, muscle relaxers, and anti-inflammatory drugs to relieve pressure and pain. Ice and cold therapies are also employed to alleviate postoperative pain and swelling. It's crucial to maintain close coordination with your surgical team when using pain medications. This ensures that the dosage and frequency of administration are accurately monitored to prevent overuse or potential side effects. Your surgical team can also advise on non-pharmacological strategies for pain management, thus providing a comprehensive approach to postoperative care.
The typical duration of recovery following spinal surgery ranges from 4 to 6 weeks, with the potential for full healing taking up to 12 weeks or even up to six months, depending on the specific type of surgery and individual circumstances.
Implementing a personalized post-surgery recovery plan, such as the Enhanced Recovery After Surgery (ERAS) program, can yield benefits in terms of reducing opioid usage, minimizing complications, and shortening the duration of hospitalization.
Summary
In conclusion, understanding different spinal surgeries and their specific uses in treating various spinal conditions can facilitate informed decisions regarding these procedures. It’s crucial to consider non-surgical treatments first, understand the benefits of minimally invasive techniques, and adequately prepare for surgery. Post-surgery, effective pain management and a personalized recovery plan can significantly enhance recovery outcomes.
Frequently Asked Questions
What is the most common spine surgery?
The most common spine surgery is spinal decompression and fusion, which is performed to relieve pressure on nerves and stabilize the spine.
What are the three types of spinal surgery?
The three types of spinal surgery are laminectomy, microdiscectomy, and traditional lumbar fusion. Laminectomy is used to treat spinal stenosis or nerve pressure in the lower back.
What is the easiest spine surgery?
The easiest spine surgery is minimally invasive spine surgery (MISS), which uses smaller incisions and causes less harm to nearby muscles and tissues, leading to less pain and faster recovery.
What is the surgery for nerves in the spine?
The surgery for nerves in the spine is a laminotomy or laminectomy, which creates space to decompress the spinal nerves and allow the nerve roots to heal. Lumbar decompression surgery is also used to treat compressed nerves in the lower spine when non-surgical treatments have not helped, aiming to alleviate persistent pain and numbness in the legs caused by nerve pressure.
What are the benefits of minimally invasive spine surgery?
Minimally invasive spine surgery provides several benefits, such as reduced muscle damage, lower infection rates, less postoperative pain, and a quicker recovery. Consider this option for a more favorable surgical experience.