Is Anesthesia Scary? Understanding and Alleviating Surgery Fears


Is anesthesia scary? This is a common concern among patients awaiting surgery. Fears of loss of control, pain, or complications may loom large. This article addresses these fears head-on, providing facts about anesthesia’s safety and strategies to cope with anxiety about surgery. By the end, you’ll have a better understanding and hopefully, less fear about your upcoming procedure.
Key Takeaways
Anxiety surrounding anesthesia, often due to fear of losing control or the unknown, can significantly affect preoperative and postoperative experiences, with potential adverse outcomes such as delayed awakening, increased pain, and longer hospital stays.
Anesthesia, particularly general anesthesia, is safer than it has ever been due to advancements in monitoring and clinical practices, with a very low risk of complications and even lower incidence rates of anesthesia-related deaths.
To alleviate concerns about anesthesia, it's important to have open communication with the healthcare team, understand the procedure and expected outcomes, and prepare for surgery by asking questions, fasting, and quitting smoking where recommended.
Learn more about other helpful strategies and how to reduce anxiety before surgery.
Unveiling the Fear Behind Anesthesia
General anesthesia, in particular, is frequently linked to preoperative anxiety. This fear can range from mild apprehension to debilitating dread, potentially affecting postoperative wound healing, pain intensity, and analgesia needs, especially in cases like trauma surgery. This fear frequently arises from common psychological triggers including:
apprehension about surgery
anesthesia
potential complications
past negative personal or family experiences with anesthetics or surgical procedures.
Unfounded beliefs and lack of proper understanding add to the fear. These may involve concerns about:
the duration of anesthesia
dread of dying during surgery
apprehension about revealing personal information under its influence
false notion of anesthesiologists leaving the room
worry about anesthesia wearing off prematurely
These concerns, although largely unfounded, can significantly impact a patient’s mental health.
The Psychology of Anesthesia Anxiety
Anxiety related to anesthesia is frequently rooted in feelings of unease, tension, and nervousness. Patients often encounter a sense of losing control, feeling vulnerable to the healthcare staff during the procedure. This fear can lead to heightened anxiety and potentially impact the patient’s surgical experience.
A significant contributor to anesthesia anxiety is the fear of losing control. Patients undergoing surgery commonly experience a general fear of the unknown, and the possibility of losing control during anesthesia can exacerbate their anxiety, especially in the operating room. Uncertainty surrounding anesthesia can intensify patients’ acute procedure anxiety and result in a range of adverse outcomes, including:
heightened anesthetic agent requirement
delayed awakening
postoperative pain
extended hospitalization.
Common Fears Associated with Anesthesia
A common fear associated with anesthesia is the worry about not regaining consciousness after its administration. However, this fear, though prevalent, is largely unfounded as the actual risk of this happening is extremely rare, at less than 1 in 100,000, making it an unwarranted fear for the majority of patients, including elderly patients.
The potential of experiencing pain during anesthesia is another prevalent fear. However, the incidence of such occurrences is relatively low, with awareness during general anesthesia happening at a rate of 1-2 per 1000 patients, and anesthesia awareness itself occurring at only 0.1-0.2%.
Allergic reactions are another concern for most patients, but they are infrequent, with significant reactions occurring in approximately 1 in 10,000 to 1 in 20,000 procedures.
The Reality of Anesthesia Risks

Contrary to common perceptions, anesthesia is generally safe and continuous advancements in technology and monitoring have made it safer than ever. The estimated perioperative complication rate ranges from 3% to 16% in industrialized nations. The protocols set in place to minimize risks during anesthesia administration include a systematic approach towards reducing risks, controlling infections, and managing patients properly to minimize potential risks.
How Safe Is General Anesthesia Today?
Regarded as safe and effective, general anesthesia carries a low risk of complications. Improvements in monitoring technology and clinical practice have been significant contributors to the enhanced safety of general anesthesia over time. However, there can be complications associated with general anesthesia, including:
Sore throat
Nausea and vomiting
Damage to teeth
Lacerations to the lips, tongue, gums, throat
Nerve injury
Cardiac arrest
Drug errors
Allergic reactions
Postoperative confusion
Heart attack
Pneumonia
Stroke
Cardiovascular changes
The current mortality rate associated with general anesthesia is as follows:
In patients without relevant systemic disease: 0.4 per 100,000
In patients with planned surgery: approximately 1 person per 100,000 general anesthetics given
Anesthesia-related death rate: 1.1 per million population per year
However, the safety of general anesthesia can be influenced by the age and health status of a patient. Older individuals and those with specific health conditions, such as heart disease, Parkinson’s disease, Alzheimer’s disease, or a history of stroke, are at a heightened risk for complications.
Comparing Local, Regional, and General Anesthesia
Depending on the procedure, local or regional anesthesia, as well as general anesthesia, each present their own set of potential benefits and risks. Local anesthesia is designed to numb a specific small area while allowing the patient to remain conscious. On the other hand, regional anesthesia is intended to numb a larger area of the body and can effectively block sensation in that specific area. Both types of anesthesia share the common effect of inducing localized numbness.
Common surgeries that typically require local anesthesia include:
Skin biopsy
Breast biopsy
Repairing a broken bone
Stitching a deep cut
Arthroscopy
Carpal tunnel release
Dental surgery
Removal of a wart, mole, or cataract
Common surgeries that typically require regional anesthesia include:
Hip and knee replacements
Certain abdominal surgeries such as hernia repair
Surgeries on the arm, wrist, or hand
Childbirth (epidural anesthesia)
On the other hand, elective surgery that necessitates patients to undergo general anesthesia includes major surgery or invasive procedures of the head, chest, or abdomen, as opposed to emergency surgery which may require immediate attention.
Preparing for Surgery: Reducing Anesthesia Concerns
Appropriate preparation and open communication with your care team can substantially alleviate concerns about anesthesia.
For a detailed guide on what to expect before surgery — including fasting instructions, common tests, and how to mentally prepare — check out our article on pre-op procedures and expectations.
Inquire with your doctors (primary care, medical specialists, surgeon, and/or anesthesiologist) about anesthesia before surgery by asking questions such as:
What is the expected wake-up time?
When can I expect to be mobile again post-surgery?
What is the anticipated duration of stay?
Will there be any post-operative pain?
What are the available anesthesia options?
How will my vital signs be monitored during the procedure?
What is the recommended operation and its necessity?
What are the alternatives to this recommended procedure?
Preoperative evaluation contributes to addressing anesthesia concerns by mitigating surgical and anesthetic perioperative morbidity or mortality, minimizing case cancellations and delays, and reducing hospital stays. Additionally, utilizing psychological preparation techniques can aid in alleviating concerns about anesthesia by minimizing post-surgery pain and enhancing behavioral recovery.
Moreover, engaging in fasting before surgery can have a beneficial impact by reducing the volume and acidity of stomach contents, which in turn helps prevent vomiting and aspiration during anesthesia. Quitting smoking, even on the day before surgery, can contribute to lowering the risk of complications.
Discussing Your Concerns with the Care Team
Maintaining open communication with your care team is of utmost importance. Expressing your fears and anxieties about anesthesia to your care team can be extremely helpful. Indeed, the anesthesia care team has the capability to modify the anesthesia plan according to the patient’s concerns and preferences. This allows the team to provide reassurance and potentially adjust the anesthesia plan to accommodate your concerns, ensuring a more comfortable and less anxiety-inducing experience.
Medications and Techniques to Ease Anxiety
Various medications and techniques are available to help reduce preoperative anxiety. Medications, such as benzodiazepines (versed and valium), are specifically formulated to reduce preoperative anxiety by lowering anxiety levels, promoting relaxation, and inducing drowsiness in preparation for surgery.
Non-pharmacological approaches such as cognitive-behavioral therapy (CBT) can also be employed. CBT has demonstrated its effectiveness in reducing preoperative anxiety for both children and adults, presenting a viable non-pharmacological approach. By understanding the nature of anxiety and employing relaxation techniques, patients can foster a more optimistic mindset prior to the procedure.
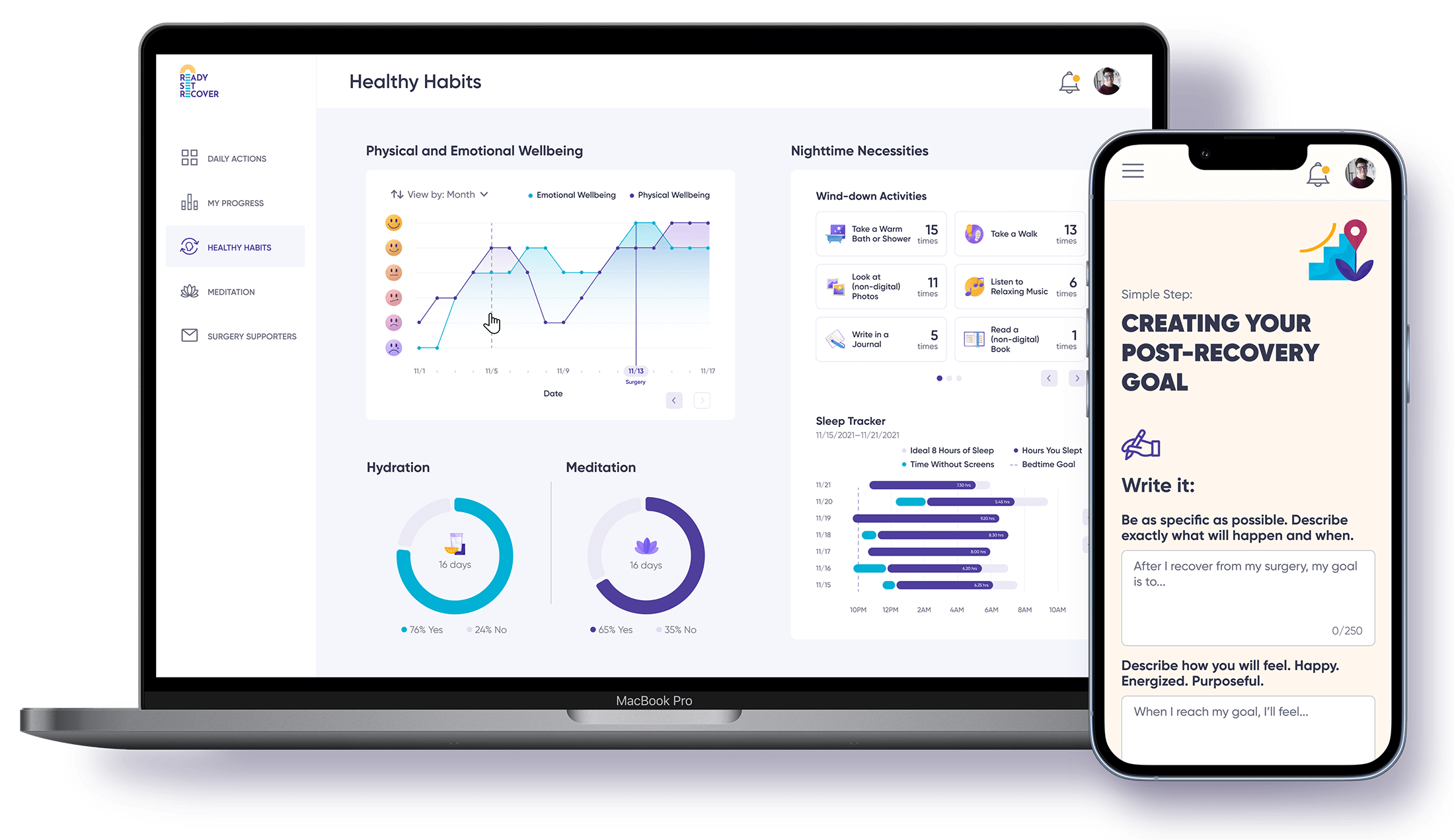
Other techniques such as using Ready Set Recover can be beneficial in reducing pre-surgery stress. Ready Set Recover is an innovative program that helps patients prepare mentally and physically for surgery. By providing a comprehensive guide of what to expect, including detailed information about the procedure, recovery process, and tips for managing post-surgery pain, it helps to alleviate fears and anxieties. This preparation can lead to a smoother surgical experience, quicker recovery, and overall improved patient outcomes.
What to Expect When Undergoing Anesthesia
Understanding what to expect during anesthesia can greatly help in lessening fears and ensuring a smoother experience. An anesthesiologist administers anesthesia by delivering a combination of medications, referred to as anesthetics, either through a mask or an intravenous (IV) line placed in the vein. Throughout the surgical procedure, the anesthesiologist is responsible for managing pain control, closely monitoring anesthesia, and monitoring vital body functions of the patient.
The dose of anesthesia is determined based on factors such as the patient’s weight, age, and overall medical status, the stimulating nature of the surgery, and individual variations in response to anesthesia.
Monitoring Vital Signs for Safety

To ensure the patient’s safety and overall health, it's crucial to monitor vital signs during anesthesia. Continuous assessment of the following is imperative for sustaining the patient’s well-being during the surgical procedure:
Oxygenation
Ventilation
Circulation
Temperature
Heart rate, blood pressure, peripheral oxygen saturation ( how well the blood is carrying oxygen to the tissues), end-tidal carbon dioxide (how well the lungs are moving carbon dioxide out of the body), and anesthesia vapor concentration are constantly monitored to evaluate the patient’s real-time condition.
Instruments such as an inflatable blood pressure cuff, a pulse oximeter, and an electrocardiogram (EKG, ECG) enable thorough monitoring of the patient’s physiological condition. Any abnormalities in vital signs, such as sudden changes, can result in serious complications such as strokes, angina, or heart attacks, underscoring the critical need for continuous monitoring to ensure patient safety.
The Process of Waking Up from Anesthesia
Waking up from anesthesia entails:
Reversing the state of total unconsciousness brought on by general anesthesia
Anesthesia care teams closely monitor the patient during this process
Making necessary adjustments in the anesthesia doses
Consistently evaluating the depth of anesthesia to prevent intraoperative awareness.
Upon awakening from anesthesia, potential side effects and complications may include:
headache
nausea
drowsiness
vomiting
sore throat caused by the breathing tube
Can I Feel Pain While Under General Anesthesia?
One question often asked by patients is if they will experience pain under general anesthesia. General anesthesia induces unconsciousness and analgesia by directly affecting the spinal cord, whereas local anesthetics block nerve signals to pain centers in the central nervous system, thus preventing the perception of pain. Pain management during and following surgery often involves:
the use of NSAIDs for mild to moderate pain
Pectoralis (chest muscle) nerve blocks to decrease postoperative pain and opioid consumption
neuraxial opioid analgesia and PCA for perioperative pain management.
During general anesthesia, the patient does not experience pain as their brain is in a state of unconsciousness and does not respond to pain signals or reflexes. Any physiological reactions the body may exhibit to pain, such as an increased heart rate or blood pressure, do not translate to the sensation of pain during surgery. Anesthesiologists endeavor to prevent intraoperative awareness and any potential sensation of pain through:
Precise drug administration
Monitoring clinical signs of any response to surgical stimulation
Avoiding overuse of muscle relaxants
Utilizing appropriate monitors throughout the procedure.
Understanding the Role of Other Drugs During Anesthesia
During anesthesia, additional drugs may be utilized to control pain, lessen anxiety, and avert complications. Supplementary medications administered during anesthesia serve to alleviate pain, alleviate anxiety, and mitigate potential complications. Sedatives play a crucial role in pacifying patients prior to a procedure, alleviating discomfort, and reducing pain and anxiety.
However, it’s important to note that drugs used in conjunction with anesthesia can lead to adverse effects, including:
Systemic and localized reactions
Excessive dosage
Rapid absorption
Inadvertent intravascular administration
Post-Anesthesia: Recovery and Aftercare

Appropriate care following anesthesia is vital for a seamless recovery and minimal discomfort. Following the administration of anesthesia, it is advisable to procure necessary medical supplies and food, ensure sufficient rest, engage in gentle movement to promote circulation, have a caregiver present for at least the initial 24 hours, and establish a secure environment by sleeping in a bedroom near a bathroom, installing night lights in hallways, decluttering, and wearing flat shoes or slippers. It is also important to remember that the first few hours after anesthesia are crucial for proper recovery.
Post-anesthesia pain management is designed to mitigate the effects of acute postsurgical pain and expedite recovery. It commonly involves the use of prescription and over-the-counter pain relievers, such as ibuprofen, acetaminophen, and aspirin. Adequate pain control following surgery can help reduce the likelihood of complications such as pneumonia and blood clots.
Additionally, managing nausea after surgery includes:
Slowly reintroducing normal foods
Favoring clear soups, mild foods, and liquids
Avoiding acidic juices and dairy products
Considering using antiemetics, to prevent vomiting, as prescribed
Ensuring adequate hydration
Managing Postoperative Pain
Addressing postoperative pain is critical for patient comfort and can be accomplished through a range of medications and techniques. Effective pharmaceutical interventions for the management of postoperative pain encompass:
Systemic pharmacologic therapy
Local anesthetic techniques
NSAIDs such as aspirin, ibuprofen, and naproxen
Opioids like codeine, fentanyl, hydrocodone with acetaminophen, hydromorphone, morphine, and oxycodone
These are all viable options for managing postoperative pain.
Variations in pain management techniques exist for different types of surgeries. Epidural analgesia (injecting pain meds into the spinal area) with a local anesthetic, an opioid, or both is considered the preferred treatment for postoperative pain control in various types of surgeries. Furthermore, the varying types of surgeries and surgical incisions can result in different types and levels of postoperative pain.
It's essential to maintain close coordination with your surgical team when it comes to the use of pain medications. This includes discussing your pain threshold, any allergies or past experiences with pain medications, and your preferences. This open communication allows the team to tailor a pain management plan that suits your specific needs and circumstances.
Tips for a Smooth Recovery at Home
Adhering to your care team’s instructions and taking good care of yourself at home can significantly contribute to a successful recovery. Here are some tips to follow:
The typical duration for complete recovery from general anesthesia at home is four to eight hours.
Engaging in walking is advisable following the administration of anesthesia.
It is important to refrain from high-impact exercises.
Adhere to the guidance provided by your physician for other physical activities.
Being vigilant for indicators of potential complications during the recuperation period is crucial. These include:
constipation
lethargy
nausea
poor appetite
pain or discomfort
difficulty breathing
swelling or redness at the surgical site
fever or chills
persistent vomiting or diarrhea
excessive bleeding or drainage
worsening pain or new pain
changes in mental status or confusion.
Scared of Anesthesia? Here’s How to Ease Surgery Fears
While the fear of anesthesia is common, understanding the process and having transparent communication with your care team can help alleviate these fears. Anesthesia, both local and general, is generally safe, with risks being minimal in most cases. Proper preparation, including mental and physical preparation, can significantly help to reduce concerns about anesthesia. After the surgery, proper post-anesthesia care and pain management are crucial for a smooth recovery. It’s important to remember that each individual’s experience with anesthesia will be unique, and understanding what to expect can help make the process less daunting.
Frequently Asked Questions
Why am I scared of going under anesthesia?
It's natural to feel apprehensive, but it's important to know that the likelihood of something going wrong under anesthesia is extremely rare, with less than a 1 in 100,000 chance of it happening. Rest assured, medical professionals take every precaution to ensure your safety during the procedure.
How do I stop being nervous about general anesthesia?
To stop being nervous about general anesthesia, it's best to talk to your perioperative team and ask them any questions you have, as they can help allay your fears. Another helpful approach is to seek information early on and talk with others about your concerns to prevent anxiety or stress.
Is it common to be afraid of not waking up from general anesthesia?
It's normal for some patients to have anxiety about not waking up from surgery or waking up during surgery, although the latter is an extremely rare phenomenon.
How does it feel to go under anesthesia?
Under general anesthesia, you should feel yourself drift off quickly, within a couple of minutes, as the anesthesia takes effect and you become unconscious. The anesthetist will ensure you stay in a controlled state of unconsciousness throughout the procedure.
How safe is general anesthesia?
General anesthesia is considered safe, with a low risk of complications. Advances in monitoring technology and clinical practice have greatly increased its safety.