Perioperative Care: Best Practices for Optimal Surgical Outcomes


Perioperative care manages patients before, during, and after surgery to reduce complications and improve recovery. This article covers best practices in perioperative medicine to enhance surgical outcomes.
Key Takeaways
Perioperative medicine employs a holistic, multidisciplinary approach to enhance patient outcomes by minimizing complications and promoting recovery throughout the surgical process.
Preoperative assessment and preparation are important for optimizing patient health, employing strategies like the Perioperative Surgical Home (PSH) and Enhanced Recovery After Surgery (ERAS) protocols to reduce risks and improve recovery.
Postoperative recovery benefits significantly from multimodal pain management and individualized care, which collectively enhance patient satisfaction and overall health outcomes.
Understanding Perioperative Medicine

The term "perioperative" is derived from the Greek prefix "peri," meaning "around" or "surrounding". In the context of perioperative medicine, this prefix aptly describes the comprehensive care provided around the time of surgery, encompassing the preoperative, intraoperative, and postoperative phases. This holistic approach ensures that patients undergoing surgery receive continuous and integrated care throughout the entire surgical process, thereby enhancing patient outcomes by minimizing complications and promoting recovery.
Good perioperative care goes beyond simply treating the surgical condition; it aims to improve the overall patient experience. It enhances the quality of care, boosts satisfaction, and reduces healthcare costs. The primary goal of the perioperative medicine team is to improve patient care throughout the perioperative period.
Consider a scenario where perioperative nurses, surgeons, anesthesiologists, and other healthcare professionals work seamlessly together. This level of coordination not only improves surgical outcomes but also significantly enhances the patient’s journey through the surgical pathway, providing better surgical care and a higher quality of life post-surgery.
Preoperative Assessment and Preparation
Preoperative assessment is the cornerstone of perioperative care. Its main objectives are to minimize surgical and anesthetic risks and ensure a quicker recovery for the patient. Optimizing a patient’s health status before surgery significantly reduces the likelihood of postoperative complications. A thorough patient history and physical examination are essential in evaluating preoperative risk factors related to cardiac and pulmonary complications.
Laboratory tests ordered based on specific patient needs, rather than routinely, help avoid unnecessary costs and interventions. Prehabilitation, a key element in the Perioperative Surgical Home (PSH) model, aims to improve the patient’s condition before surgery. The PSH model optimizes patient health and surgical care while reducing costs.
Enhanced Recovery After Surgery (ERAS) protocols are also a common component of preoperative care. These protocols standardize care and improve outcomes for surgical patients. A targeted program that addresses nutrition, physical activity, and psychological issues is essential for prehabilitation in preoperative care. This comprehensive approach ensures that patients are in the best possible shape to undergo surgery, thereby enhancing the overall surgical experience and outcomes.
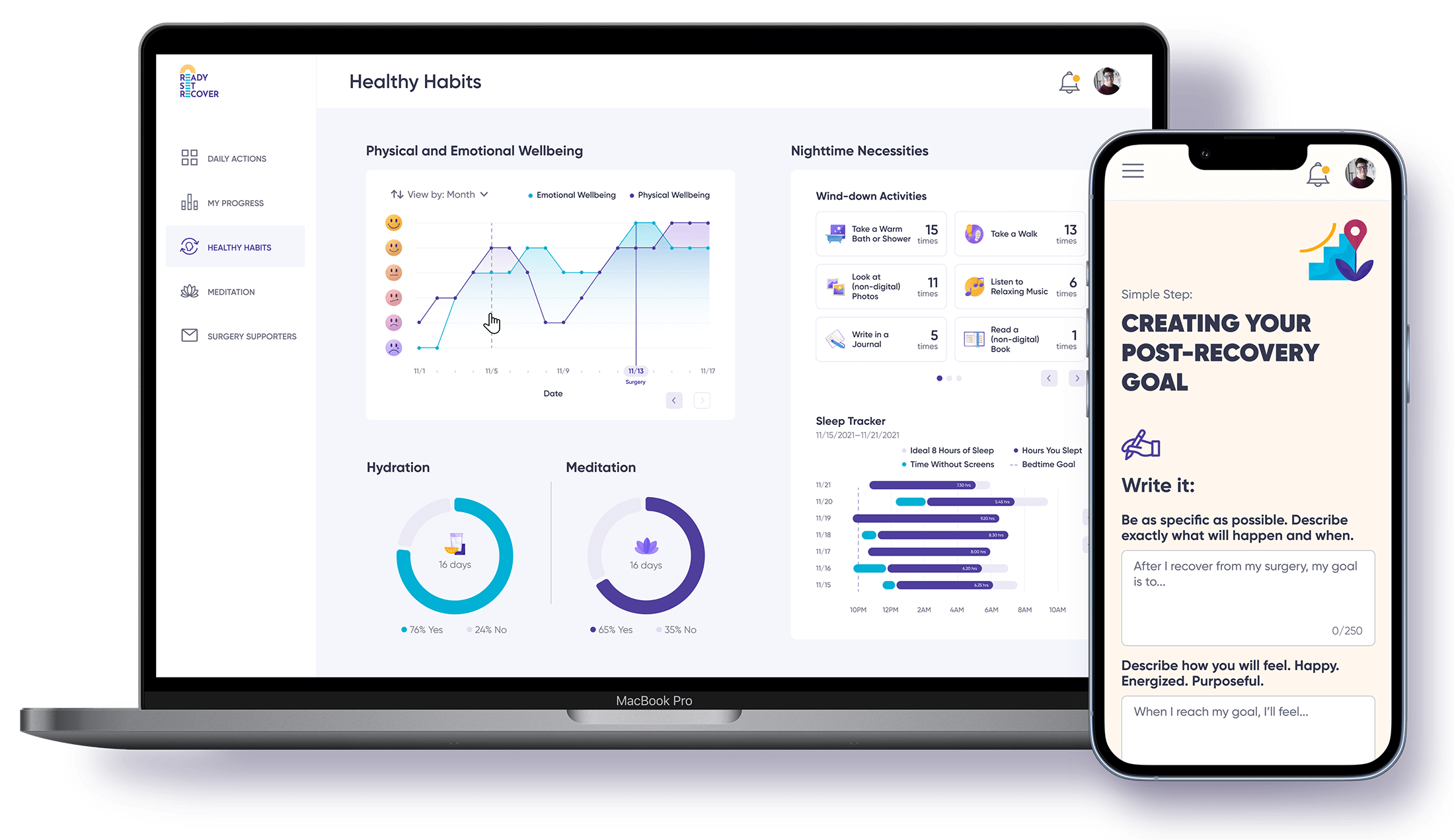
Programs like Ready Set Recover play a vital role in preparing patients for their upcoming surgeries. By providing tailored advice and resources, such programs guide patients through the preoperative process, helping them understand what to expect and how to optimize their health before the procedure. This preparation can greatly enhance patient confidence and contribute to better surgical outcomes.
Intraoperative Care and Management

Intraoperative care refers to the specialized medical attention and management provided to patients during a surgical procedure. This critical phase of perioperative care involves the expertise of anesthesiology clinicians who ensure patient safety, effective pain management, and the maintenance of vital functions throughout the surgery. Intraoperative care also includes monitoring the concentration of anesthetic agents and coordinating with the surgical team to prevent complications, thereby enhancing the overall surgical process and patient outcomes. is where the expertise of anesthesiology clinicians shines. They provide specialized care during surgical procedures, ensuring patient safety and effective pain management. One important aspect of their role is monitoring the concentration of anesthetic agents to prevent accidental awareness during surgery.
Accidental awareness during general anesthesia, although rare, can have significant implications. The incidence ranges from 1 in 1,000 to 1 in 20,000, with certain factors such as the use of muscle relaxants increasing this risk. Emergency surgeries, which often require rapid anesthetic induction, can compromise the depth of anesthesia and increase the risk of awareness. Effective coordination within the perioperative team can enhance patient safety and streamline the surgical process.
Patients with a history of intraoperative awareness may have a higher risk of experiencing awareness during subsequent surgeries. This requires the surgical team to thoroughly plan and manage anesthesia, taking all possible precautions to maintain patient safety and comfort throughout the operation.
Postoperative Recovery and Follow-up

The journey to recovery doesn’t end when the surgery is completed. Postoperative recovery is an essential phase where the implementation of Enhanced Recovery After Surgery (ERAS) protocols can lead to significant reductions in postoperative complications. ERAS protocols emphasize multimodal pain management strategies, often preferring NSAIDs over opioids to facilitate recovery.
Pain management is not just about alleviating physical discomfort; it is a large aspect of the overall patient’s health experience, impacting both recovery and satisfaction levels. Patients often express a strong need for psychological support during recovery, highlighting the major impact of mental well-being on overall experiences. Considering personal and family circumstances leads patients to report a more positive perioperative experience.
Providing information about pain management options helps patients feel more in control and reduces anxiety after surgery. Individualized care addressing specific patient needs can alleviate anxiety and foster better adherence to treatment protocols. Collaborative care models help reduce variations in treatment and enhance the overall quality of care in surgical settings.
High-quality perioperative care reduces perioperative complications, shortens the length of stay, improves experience, and can result in cost savings.
Integrated Perioperative Services

Perioperative care is a multidisciplinary approach that emphasizes collaboration among various healthcare professionals for optimal patient outcomes. Perioperative nurses play a large role in surgical teams, ensuring patient safety and comfort throughout the surgical process. Education and training for these nurses often require a Bachelor of Science in Nursing and specialized certification in perioperative care.
Both the Perioperative Surgical Home (PSH) and Enhanced Recovery After Surgery (ERAS) models are integrated to enhance care delivery for patients with complex medical conditions. Standardized ERAS guidelines have been established for a variety of surgical procedures to enhance recovery. The integration of PSH and ERAS facilitates the management of patients with chronic diseases during the perioperative phase.
Effective coordination and clear communication between health care providers directly affect patient satisfaction and recovery outcomes. Collaboration, investment, education, and a cultural shift are essential to transforming the delivery of future perioperative care. Current research emphasizes the use of technology and data science to improve patient outcomes.
Research and Innovation in Perioperative Medicine
Research in the field focuses on identifying risk factors or problems around the time of surgery. Studies investigate the impact of physiological disruptions during surgery on various organ systems. Enhancing patient monitoring during and after surgery is a key research area to ensure safety and better outcomes.
Artificial intelligence and machine learning are explored for applications like risk assessment and improving clinical workflows. The study of perioperative medicine is experiencing new insights and significant advancements due to recent scientific achievements. These innovations promise to revolutionize perioperative care, offering better surgical care and improving patient experience.
Enhancing Patient Experience
Enhancing patient experience is essential throughout the perioperative pathway, as it directly influences surgical outcomes and patient satisfaction. Mobile health technologies are being employed to enhance patient education and gather health data related to surgical care.
Effective perioperative care enhances patient satisfaction, improves overall health outcomes, and reduces healthcare costs. When healthcare professionals consider personal and family circumstances, patients report a more positive perioperative experience, emphasizing the importance of individualized care.
Addressing New Challenges in Perioperative Care
The surgical patient population is growing, with over 310 million surgeries performed annually worldwide, necessitating improved perioperative services in the surgical ward. One of the major challenges facing perioperative care is the need to adapt to the increasing complexity of patient conditions and surgeries.
Interdisciplinary collaboration has been key for research efforts, especially in evaluating surgical safety. As the demand for surgeries increases, perioperative medicine must evolve to address these new challenges, ensuring that patients receive the highest standard of care.
Summary
Perioperative care is an essential component of the surgical process, encompassing everything from preoperative assessments to postoperative recovery. Its multidisciplinary, patient-centered approach ensures that patients receive the highest standard of care, improving outcomes and satisfaction.
By integrating the latest research, innovative practices, and personalized care plans, perioperative medicine continues to evolve, meeting the challenges of a growing and increasingly complex surgical patient population. With continued collaboration and investment, the future of perioperative care looks promising.
Frequently Asked Questions
What is the main goal of perioperative medicine?
The main goal of perioperative medicine is to improve patient outcomes by preventing complications and facilitating recovery through a multidisciplinary and patient-centered approach.
How does preoperative assessment help in surgery?
Preoperative assessment is important because it minimizes surgical and anesthetic risks while optimizing the patient's health, leading to quicker recovery. This process ensures a safer surgical experience overall.
What are ERAS protocols?
ERAS protocols are standardized guidelines aimed at enhancing patient outcomes and promoting quicker recovery following surgical procedures. Implementing these protocols can significantly improve overall surgical recovery experiences.
How do perioperative services integrate different healthcare professionals?
Perioperative services effectively integrate different healthcare professionals through a multidisciplinary approach that fosters collaboration among nurses, surgeons, anesthesiologists, and others, ensuring optimal patient outcomes. This coordinated teamwork is essential for successful surgical procedures and patient care.
What role does research play in perioperative medicine?
Research plays a pivotal role in perioperative medicine by identifying risk factors and enhancing patient monitoring, which ultimately improves clinical workflows and patient outcomes. This focus on continuous improvement is essential for advancing patient care in surgical settings.