What Are the Chances of Dying During Surgery? Risk Factors

Worrying about the risk of dying during surgery is natural, and many patients have this fear before a procedure. While the odds of dying during surgery are low, especially for planned, elective surgeries, understanding the risks involved and the factors that affect those risks can provide some much-needed reassurance. This article aims to explore the risk of dying during surgery, focusing on different risk factors and the measures that can help make surgeries safer.
Understanding Postoperative Mortality
Understanding postoperative mortality is essential for evaluating surgical risks and outcomes. But what are the chances of dying during surgery? One key factor is postoperative mortality, which refers to the likelihood of a patient dying within a set period after surgery, typically within 30 days. This timeframe is critical, as patients face the highest risk of complications related to the procedure or anesthesia. Understanding postoperative mortality helps assess surgical success and overall healthcare quality.
What is Intraoperative Mortality?

Intraoperative mortality refers to deaths that occur during the surgical procedure itself, while the patient is in the operating room. Intraoperative mortality is influenced by factors such as the patient’s health status, the complexity of the surgery, and the experience of the surgical team.
In the United States, intraoperative mortality is relatively rare, occurring in approximately 3.3 per 10,000 surgeries, or 0.033% of cases. This rate includes both elective and emergency surgeries. However, the risk is significantly higher for emergency surgeries compared to elective procedures. Elective surgeries benefit from detailed preoperative planning and patient optimization, leading to a lower intraoperative risk. Conversely, emergency surgeries are performed under urgent conditions, often without sufficient time to stabilize the patient, which increases the likelihood of intraoperative complications and mortality.
30-Day Postoperative Mortality Rates
The risk of dying after surgery also varies depending on several factors such as the type of surgery, the patient’s overall health, and the urgency of the procedure. For elective surgeries, the risk is generally very low because the patient’s health can be optimized beforehand, and the procedure is well-planned. In the United States, the 30-day mortality rate for elective surgeries is approximately 0.67%, which aligns with more recent studies that indicate a slightly higher figure than previously reported.
The overall 30-day postoperative mortality rate in the United States, which includes both elective and emergency surgeries, is estimated to be around 1.89%. This figure is influenced by the inclusion of high-risk emergency procedures, which significantly increase the overall average. Emergency surgeries carry a substantially higher risk, with the 30-day mortality rate in the U.S. around 3.7%. This increased risk is largely attributed to the urgent need for immediate intervention, the unstable condition of many patients, and the presence of multiple health complications that often accompany emergency procedures.
Global Perspective

Globally, postoperative mortality is a major concern. According to the World Health Organization (WHO), approximately 4.2 million people die within 30 days of surgery each year, representing an estimated 1.34% of the 313 million surgical procedures performed annually. Alarmingly, half of these deaths occur in low- and middle-income countries (LMICs), despite these countries accounting for only a small fraction of all surgeries performed globally. In fact, LMICs perform approximately 3.5% of the world's surgeries, yet they account for half of all postoperative deaths. This stark imbalance highlights significant disparities in healthcare access, surgical quality, and overall patient outcomes between LMICs and high-income countries. Factors such as limited resources, inadequate surgical infrastructure, and a shortage of trained healthcare professionals contribute to these higher mortality rates. Recognizing the factors that lead to postoperative mortality is vital for improving surgical outcomes and decreasing the likelihood of death following surgery.
Globally, intraoperative and postoperative mortality rates vary based on healthcare infrastructure, patient population, and the complexity of procedures:
In high-income countries (HICs), elective surgeries generally have a lower perioperative mortality rate, often less than 1%, while emergency surgeries can reach up to 4-5% in terms of 30-day postoperative mortality. Additionally, high-income countries often have more robust healthcare systems that allow for better preoperative care, early detection of complications, and access to critical care facilities, which collectively contribute to lower mortality rates.
In low- and middle-income countries (LMICs), both elective and emergency surgeries carry higher risks due to limited resources, less access to advanced medical technologies, and fewer opportunities for preoperative optimization. The lack of adequately trained surgical staff and the scarcity of essential medical supplies also contribute to increased mortality rates. Studies have found that up to 20% of surgical patients in LMICs may develop serious complications, and the probability of mortality is significantly heightened compared to HICs.
The WHO also notes that a significant proportion of people in LMICs do not have access to safe surgery. Expanding access to quality surgical care, improving healthcare infrastructure, and investing in preoperative and postoperative care are crucial steps towards reducing these global disparities in surgical outcomes.
Key Risk Factors Influencing Surgical Outcomes
1. Underlying Health Conditions
Chronic diseases such as congestive heart failure, diabetes mellitus, and chronic obstructive pulmonary disease (COPD) are among the major risk factors that can influence surgical outcomes. The presence of these conditions can increase the likelihood of complications both during and after surgery. Identifying and managing these conditions beforehand can significantly improve patient outcomes and reduce postoperative morbidity.
2. Age, Gender and Physical Status
The patient's age is a major risk factor in surgical outcomes. Older patients are particularly susceptible to adverse outcomes due to decreased physiological reserves and the presence of multiple comorbidities. As age increases, the body's ability to recover from surgical stress diminishes, leading to a higher risk of complications and postoperative mortality. The American College of Surgeons provides guidelines to assess a patient's overall health and readiness for surgery, which are particularly important for elderly patients. This comprehensive evaluation helps in predicting potential risks and tailoring interventions to enhance recovery and improve clinical outcomes for older individuals undergoing surgery.
Gender also plays a role in surgical outcomes, with studies indicating that male patients often face a higher risk of postoperative complications and mortality compared to female patients. This disparity may be attributed to differences in hormonal profiles, immune response, and the prevalence of certain risk factors like coronary artery disease, which are more common in men. Furthermore, gender differences in pain perception and recovery rates can influence patient outcomes. Understanding these gender-specific factors is crucial for tailoring surgical care and improving postoperative recovery for both male and female patients.
Functional status is another significant factor that influences surgical outcomes. Patients with limited mobility or those who require assistance in daily activities face a greater risk of postoperative morbidity and mortality. A thorough assessment of functional status allows healthcare providers to implement strategies that can enhance recovery, such as physical therapy and nutritional support. By addressing these factors, medical teams can tailor perioperative care to improve patient outcomes and reduce the risk of adverse events during and after the surgical procedure.
3. Type of Surgery: Elective vs. Emergency
Elective surgeries are medical procedures that are planned in advance and are not considered emergencies. These surgeries are typically scheduled at a convenient time for both the patient and the medical team, allowing for thorough preoperative assessment and preparation. Elective surgeries can range from minor procedures, such as removing a mole, to more complex operations like joint replacements or cosmetic surgeries.
Because elective surgeries are planned, they generally pose a lower risk compared to emergency surgeries. This is primarily because there is ample time to optimize the patient's health before the procedure, manage any existing health issues, and ensure the surgical team is fully prepared. The ability to plan and prepare significantly reduces the likelihood of complications and improves surgical outcomes.
On the other hand, emergency surgeries carry a higher risk due to their urgent nature. These procedures often need to be performed immediately to address life-threatening conditions or severe injuries, leaving little time to manage existing health issues. Emergency general surgeries, in particular, tend to have higher postoperative morbidity and mortality rates, significantly affecting patient outcomes, especially for high-risk patients.
4. Type and Complexity of Surgery
The type and complexity of the surgery are crucial factors that significantly affect the risk of death during surgical procedures. Major surgeries, such as cardiac or complex abdominal surgeries, inherently carry a higher risk compared to minor procedures. This increased risk is due to the extensive nature of these operations, which often involve critical organs and require longer operative times. These factors elevate the potential for surgical complications, such as blood loss, infection, and postoperative morbidity.
Complex surgeries also demand a higher level of expertise and precision from the surgical team. The involvement of multiple specialists and advanced surgical techniques can mitigate some risks, but the inherent complexity still presents challenges.
5. Smoking Status and Preoperative Preparation
Smoking status also plays a significant role in determining the risk of complications during surgery. Smokers face a higher risk of both respiratory failure and surgical site infections. Medical professionals typically advise patients to quit smoking well before surgery to lower these risks and improve their chances of a successful recovery.
6. Operative and Cardiac Risk Factors
Cardiac risk factors are also a major concern. Conditions such as coronary artery disease and a history of myocardial infarction can increase the risk of death during surgery. Assessing these operative risk factors early allows healthcare providers to take necessary precautions, such as involving a cardiologist in preoperative care to optimize heart function.
7. Medications
The use of medications, particularly anticoagulants and antiplatelet agents, can complicate surgical procedures by increasing the risk of bleeding. A careful review of a patient's medication regimen is key to balancing the benefits and risks associated with their use.
Ultimately, a multidisciplinary approach that involves surgeons, anesthesiologists, cardiologists, and other specialists is often necessary to optimize a patient's condition before surgery. This collaborative effort ensures that all potential risk factors are addressed, leading to better surgical outcomes and reduced postoperative mortality.
8. The Surgeon and the Hospital
Lastly, the choice of a surgeon can influence the risk of dying during surgery. Not all surgeons possess the same level of expertise, and their experience with specific procedures can greatly affect surgical outcomes. Surgeons who have extensive experience and specialized training in a particular type of surgery are often more adept at handling complex cases and unforeseen complications, thereby reducing the risk of adverse outcomes.
Experience vs. Inexperience: A surgeon's experience with a specific procedure is paramount. Those who frequently perform a particular surgery are more likely to have refined their techniques and developed a strong understanding of potential complications. In contrast, less experienced surgeons may not possess the same level of skill or familiarity, potentially increasing the operative risk factors and the likelihood of surgical complications.
Training and Credentials: The training and credentials of a surgeon also play a significant role. Surgeons who have trained at prestigious institutions or have completed fellowships in specialized fields may have access to advanced techniques and cutting-edge knowledge, which can enhance patient outcomes. Additionally, board certification and membership in professional organizations, such as the American College of Surgeons, indicate a commitment to maintaining high standards of surgical care.
Location of Surgery: Where the surgery is performed can also impact the risk. Hospitals with better reputations, often associated with higher volumes of specific surgeries, tend to have more comprehensive resources and support systems in place. These facilities may offer state-of-the-art technology, specialized surgical teams, and rigorous safety protocols, all of which contribute to improved surgical outcomes. Conversely, surgeries performed in less reputable or international locations may not adhere to the same standards, potentially increasing the risk of postoperative complications and mortality.

Multidisciplinary Approach: A surgeon who collaborates with a multidisciplinary team, including anesthesiologists, cardiologists, and other specialists, can provide more comprehensive care. This collaborative approach ensures that all aspects of the patient's health are considered, and potential risk factors are addressed, leading to better clinical outcomes.
In conclusion, the surgeon's expertise, training, and the location of the surgery are pivotal factors that can significantly influence the risk of death during surgery. By choosing a highly experienced surgeon and a reputable hospital, patients can enhance their chances of a successful surgical outcome and reduce the risk of postoperative mortality.
Common Complications and How to Mitigate Them
Postoperative complications like surgical complications, infections, blood clots, and respiratory issues are common after major surgery. Surgical patients with underlying health conditions are particularly susceptible. Careful monitoring during the immediate postoperative period is important in identifying any adverse events early and improving surgical outcomes. This also plays a role in minimizing adverse outcomes and improving the overall clinical outcomes for high-risk patients.
Postoperative Pulmonary Complications
Pulmonary complications, such as respiratory failure, are often seen in patients with pre-existing lung conditions or those undergoing major surgeries. Ensuring proper perioperative care, including respiratory exercises and monitoring by specialists, can significantly reduce these risks.
Preventing Surgical Site Infections
Surgical site infections are a significant source of postoperative morbidity. Maintaining a sterile environment, using surgical soap during preparation, and administering preventive antibiotics can greatly minimize this risk. Patients are also encouraged to follow all preoperative preparation guidelines to ensure a cleaner surgical site.
Measures Taken by the Medical Community to Reduce Risks
1. Comprehensive Preoperative Assessment
The American College of Surgeons emphasizes the importance of preoperative assessment, which includes evaluating risk factors such as smoking status, cardiac health, and overall fitness level. A detailed preoperative evaluation can identify high-risk patients and help tailor the surgical care plan to minimize adverse outcomes. This helps improve clinical outcomes and reduces the incidence of postoperative complications.
2. Use of Enhanced Recovery Protocols
Enhanced recovery protocols (ERPs) are increasingly being adopted to improve surgical outcomes, reduce postoperative morbidity, and minimize overall mortality rates. ERPs involve a combination of pain management, nutrition optimization, and physical activity to help patients recover faster and reduce complications. These protocols have proven to be particularly effective in major surgeries.
3. World Health Organization Surgical Safety Checklist
The World Health Organization (WHO) has developed a surgical safety checklist aimed at reducing complications and deaths occurring during surgery. This checklist covers preoperative, intraoperative, and postoperative steps, ensuring that no measures are overlooked. The use of this checklist has been shown to significantly reduce surgical morbidity and mortality rates.
Managing Anxiety About Surgical Risks

It is completely normal to feel anxious about the possibility of dying during surgery. Anxiety can be a difficult aspect to manage, but there are several strategies to help ease your concerns:
Talk to Your Healthcare Provider: One of the most effective ways to alleviate anxiety is to have an open and honest discussion with your surgeon about your concerns. Surgeons are accustomed to addressing patient anxieties and can provide valuable insights into the specific measures being taken to ensure your safety. By discussing your worries, you can gain a clearer understanding of the surgical procedure, the associated risks, and the steps being implemented to mitigate those risks. This dialogue not only helps in demystifying the surgical process but also empowers you to make informed decisions about your health care. Remember, your surgical team is there to support you, and addressing your concerns openly can foster a sense of trust and confidence in your surgical journey.
Practice Relaxation Techniques: Techniques such as deep breathing exercises, meditation, or progressive muscle relaxation can help manage anxiety in the days leading up to your surgery. These practices can help calm your nervous system and make it easier to cope with stress. Engaging in these relaxation techniques not only aids in reducing anxiety but also contributes to overall well-being. Deep breathing exercises can enhance oxygen flow, promoting better circulation and helping you maintain a sense of calm. Meditation encourages mindfulness, allowing you to focus on the present moment and alleviate worries about the future. Progressive muscle relaxation involves tensing and then slowly releasing each muscle group, which can relieve physical tension and promote relaxation. Incorporating these techniques into your daily routine can create a positive habit that supports both mental and physical health, ultimately preparing you for a smoother surgical experience.
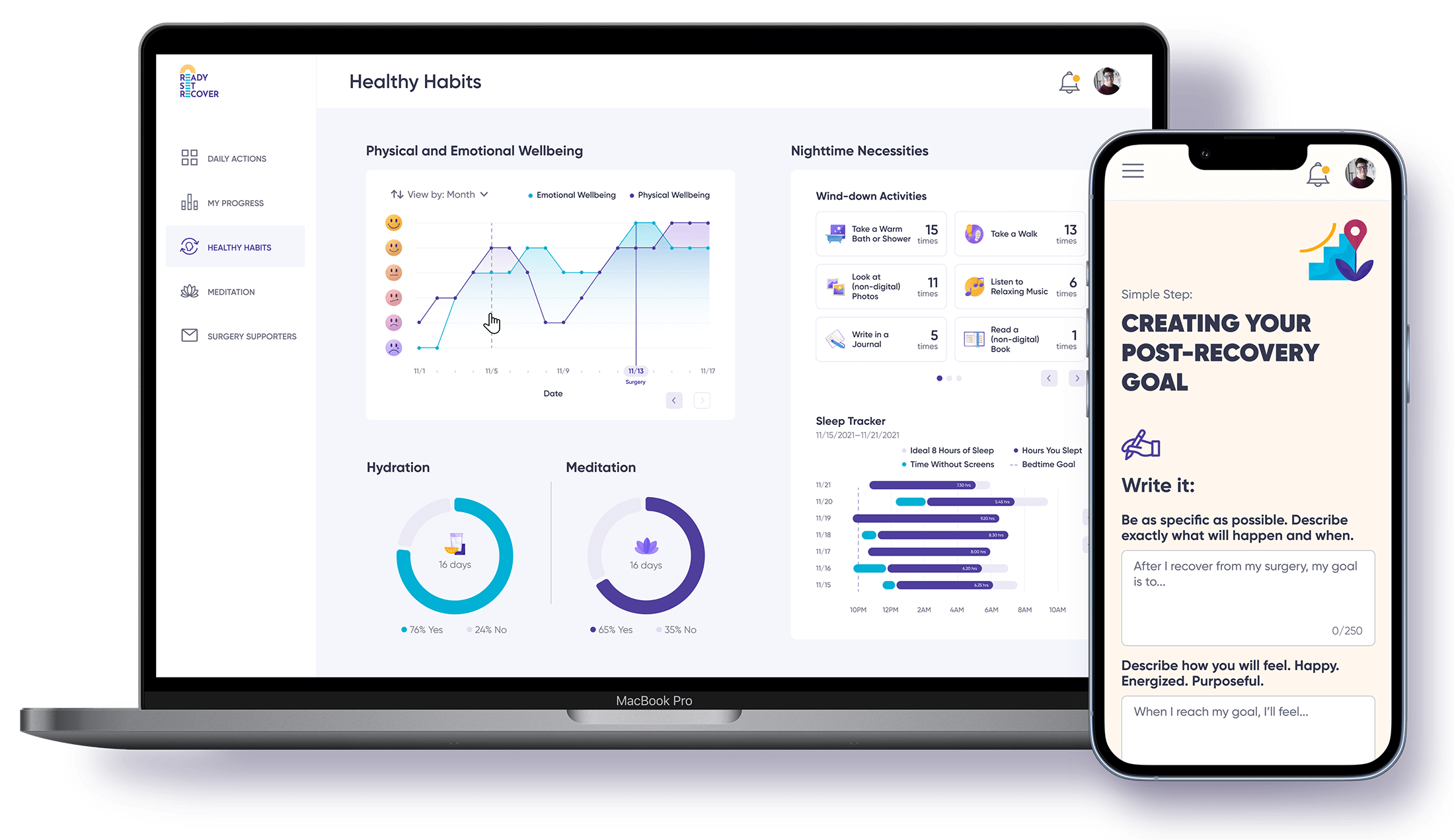
Consider Support Programs Like Ready Set Recover: Ready Set Recover is an innovative platform designed to empower patients through the surgical process. It provides a structured program to help you prepare both physically and mentally for surgery, offering holistic tools to reduce anxiety and improve recovery. With educational resources and practical guidance, Ready Set Recover can give you a greater sense of control and confidence in your surgical journey.
Join a Support Group: Speaking to others who have undergone similar surgeries can be very helpful. Many hospitals and clinics have support groups or peer mentors who can provide personal insights and advice based on their experiences. These groups offer a platform for sharing stories, discussing fears, and exchanging tips on how to cope with anxiety before and after surgery. Engaging in these communities can foster a sense of camaraderie and understanding, as members often share similar concerns and experiences. Support groups can also be a source of practical advice, such as how to manage postoperative pain or tips for a smoother recovery. Additionally, these groups can help you feel less isolated in your journey, knowing that others have faced and overcome similar challenges. The emotional support and encouragement from peers can be incredibly comforting and empowering, helping you build resilience and confidence as you prepare for your surgical procedure.
Therapy and Counseling: Therapy and Counseling: If anxiety is overwhelming, consider speaking to a therapist who specializes in medical anxiety. Cognitive Behavioral Therapy (CBT) can be effective in addressing specific fears related to surgery and providing strategies to reframe anxious thoughts. CBT works by helping individuals identify and challenge negative thought patterns and beliefs, replacing them with more balanced and realistic perspectives. Through CBT, patients can learn relaxation techniques, develop coping strategies, and gradually reduce their anxiety levels. Additionally, therapy can provide a safe space to explore any underlying concerns or past experiences that may be contributing to the anxiety, allowing patients to gain a deeper understanding of their emotions and develop personalized strategies for managing them. Engaging in therapy before surgery not only helps in reducing anxiety but also equips patients with valuable tools for handling stress in other areas of life, ultimately enhancing overall well-being.
Focus on Positive Outcomes: Remind yourself of the reasons why the surgery is necessary and the positive outcomes it can bring. Focusing on the benefits rather than the risks can help shift your mindset toward a more positive perspective. Consider the improvements in your quality of life, such as reduced pain, enhanced mobility, or the management of a chronic condition that the surgery aims to address. Visualizing these positive changes can be a powerful motivator, helping you maintain a hopeful outlook throughout the surgical process. Additionally, acknowledging the expertise and experience of your surgical team can further bolster your confidence in achieving a successful outcome. By concentrating on the potential for a better future, you empower yourself to face the procedure with courage and optimism, ultimately contributing to a more positive surgical experience.
Managing anxiety is an important aspect of preparing for surgery, and using the right tools and support systems can make a significant difference in your mental and physical well-being.
What Are the Chances of Dying During Surgery? Reducing the Risk
While the thought of dying during surgery can be daunting, understanding the risks involved and taking active measures to mitigate those risks can help reduce anxiety. Modern surgical care has advanced significantly, with a focus on reducing mortality, minimizing adverse outcomes, and improving overall clinical outcomes for patients undergoing surgery. By adhering to preoperative guidelines, communicating openly with healthcare providers, and understanding your specific risk factors, you can take important steps toward ensuring a safe surgical experience.
Frequently Asked Questions
Is It Normal to Worry About Dying During Surgery?
Absolutely. It is common to feel anxiety about the risks associated with surgery. Discussing these concerns with your healthcare provider can help you understand the steps being taken to minimize these risks and provide some peace of mind.
What Are the Odds of Survival from Surgery?
The odds of survival are generally very high for elective surgeries, especially when performed on relatively healthy patients. The mortality rate is significantly lower for planned procedures compared to emergency surgeries.
What Are the Top 3 Riskiest Surgeries?
The top three riskiest surgeries are generally major heart surgery, complex abdominal surgery performed in emergency settings, and surgeries involving major trauma. These surgeries have higher risks due to the complexity and the underlying health status of patients needing them.
What Are the Risk Factors for Dying Under Anesthesia?
Risk factors for dying under anesthesia include advanced age, existing health conditions like coronary artery disease, poor functional status, and emergency surgery. Proper preoperative evaluation can help mitigate these risks.
What is the riskiest surgery?
The riskiest surgeries include open-heart surgery, brain surgery, and organ transplants, due to their complexity and potential complications. Emergency surgeries and procedures for high-risk patients also have higher mortality rates.
What is the hernia surgery risk of death?
The risk of death from hernia surgery is very low, typically less than 0.5%, but it increases in older adults, those with severe health conditions, or in emergency cases where the hernia is strangulated.
What is the pacemaker surgery mortality rate?
The mortality rate for pacemaker surgery is low, generally under 1%, though risks increase with age, existing heart conditions, or complications like infections or bleeding.
Why do people die during cosmetic surgery?
Deaths during cosmetic surgery often result from anesthesia complications, blood clots, underlying health issues, or unqualified surgeons. High-risk procedures like Brazilian butt lifts (BBLs) have a higher mortality rate, due to fat embolism risks.